Super Flu on the Rise Across the US: What You Need to Know

‘Super Flu’ Cases Rising Across US: What to Know
Reports of a severe influenza variant, dubbed the ‘super flu,’ are surging nationwide as subclade K of influenza A H3N2 dominates this season. Originally noted in the UK, this mutated strain has crossed the Atlantic, driving high case counts in states like New York, Rhode Island, and Colorado, with the CDC logging millions of illnesses, thousands of hospitalizations, and over 1,200 deaths so far[2][4]. Unlike typical flu, it hits harder and lingers longer, fueled by lower population immunity since H3N2 hasn’t led recent seasons[5].
Symptoms and Progression
Symptoms strike suddenly: high fever, chills, intense headaches, sore throat, muscle aches, dry cough, profound fatigue, and brain fog within hours[1]. The onset phase (days 1-2) brings exhaustion; peak (days 2-5) worsens with severe pain, poor sleep, nausea, and vomiting especially in children[1][3]. Recovery drags beyond standard flu, pressuring health systems amid holiday spreads[3]. High-risk groups like seniors, pregnant individuals, and those with conditions face elevated severity[5].
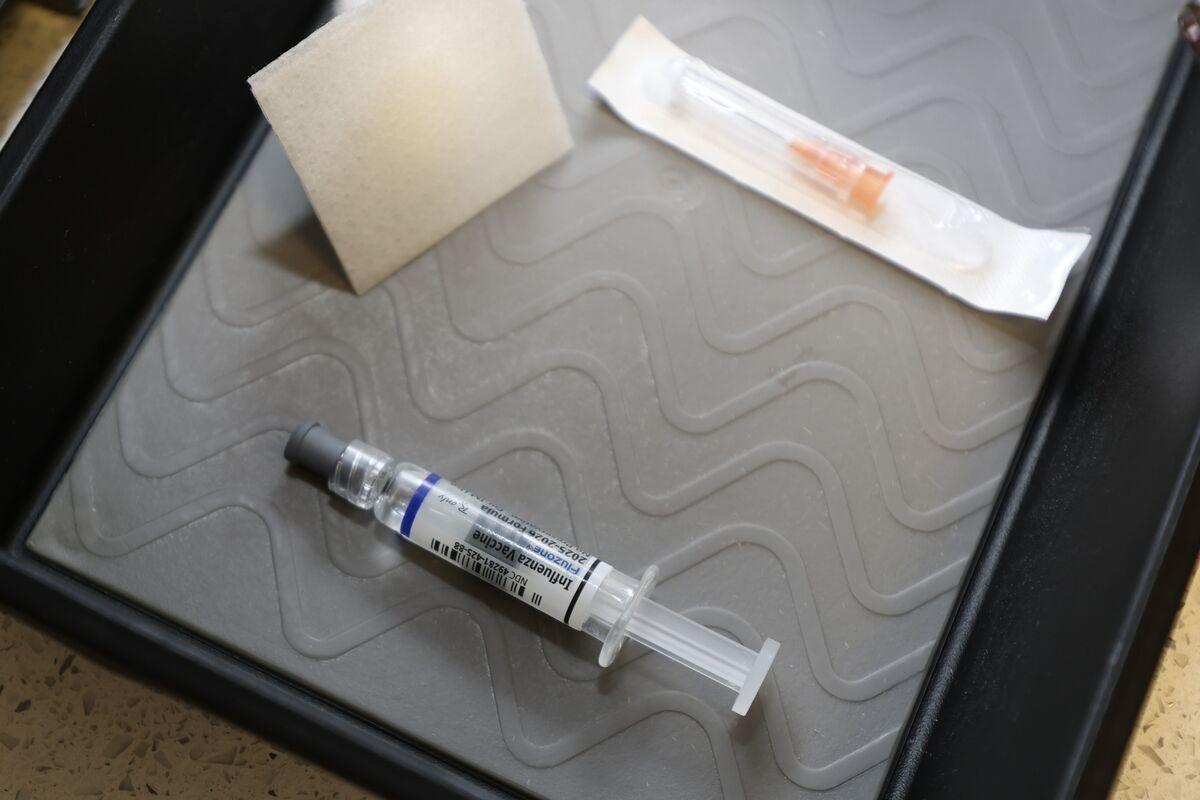
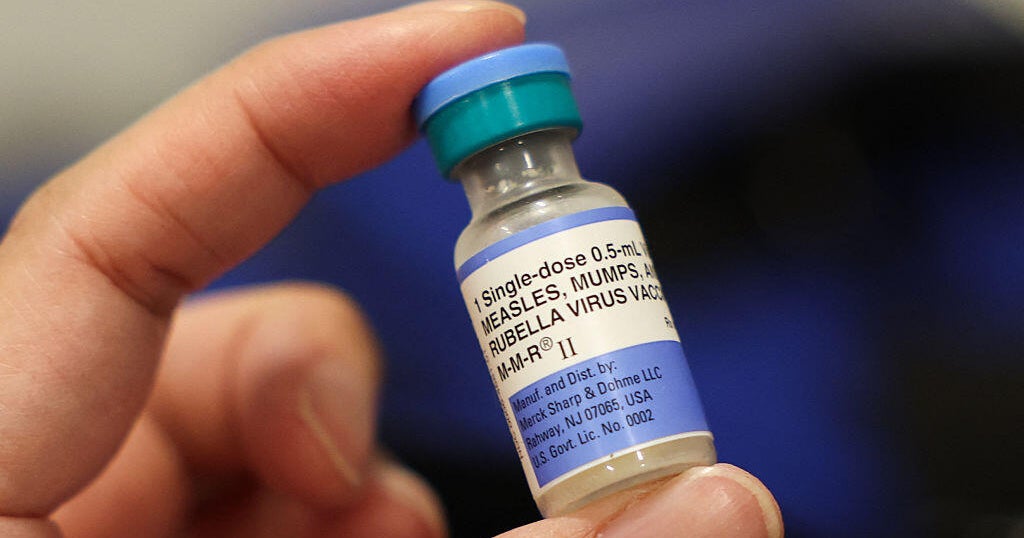
Protection and Treatment
The flu vaccine offers solid defense—32-39% effective in adults, up to 75% in kids against severe cases[4]. Antivirals like Tamiflu work best within 48 hours; home tests for flu and COVID aid quick action[2][3]. Prevent spread via handwashing, disinfecting surfaces, and masking in crowds. Health officials urge eligible vaccination now, as peaks may hit February[3][6]. Stay vigilant this intense season.
About the Organizations Mentioned
CDC
The **Centers for Disease Control and Prevention (CDC)** is the premier national public health agency of the United States, operating under the Department of Health and Human Services and headquartered in Atlanta, Georgia. Its primary mission is to protect public health and safety through disease control, injury prevention, and health promotion both nationally and globally[1][8]. Established in 1946 initially as a single "Center for Disease Control," the agency expanded and reorganized in 1980 into multiple specialized centers, reflecting a broader focus beyond infectious diseases to include environmental health, chronic disease, occupational safety, and health education[7]. The CDC comprises various centers and institutes, such as the National Center for Immunization and Respiratory Diseases, the National Center for Chronic Disease Prevention and Health Promotion, and the National Institute for Occupational Safety and Health (NIOSH), among others. These centers enable the CDC to address a wide array of public health challenges through research, surveillance, policy development, and education[2]. It also plays a key role in emergency preparedness and response, demonstrated notably during the COVID-19 pandemic, where its guidance shaped public health actions despite complex political and social dynamics[8]. Key achievements include pioneering epidemiological research, controlling outbreaks of infectious diseases, advancing vaccine safety and immunization programs, and addressing emerging health threats such as obesity and diabetes. The CDC is recognized for disseminating authoritative health information, including the widely cited Morbidity and Mortality Weekly Report (MMWR), and for its global collaborations with health organizations worldwide[1][3][8]. Currently, the CDC is undergoing organizational adjustments to focus more intensively on infectious diseases, as part of the 2025 Department of Health and Human Services reorganization. This includes absorbing the Administration for Strategic Preparedness and Response while shifting some functions like occupational safety to new entities[1]. The agency’s comprehensive approach, backed by science and government funding, positions it as a critical leader in public health innovation, disease prevention, and health security i