Why Flu Season Is So Bad This Year: The Subclade K H3N2 Outbreak

Why Is Flu Season So Bad This Year?
This year's flu season in the U.S. is hitting harder than expected, with the CDC reporting at least 18 million illnesses, 230,000 hospitalizations, and over 9,300 deaths so far.[1][2] Respiratory illness visits remain high in 33 states, marking one of the most severe outbreaks in recent years.[1]
The Culprit: Subclade K of H3N2
A new branch on the flu family tree, subclade K—a variant of the H3N2 influenza A virus—is driving most cases.[1][5] This strain evaded full prediction during last year's vaccine selection, leading to intense circulation seen in Australia's prolonged season and early surges in Hong Kong and New York.[5] Hospitals report flu admissions dwarfing COVID and RSV cases, overwhelming emergency departments.[3]
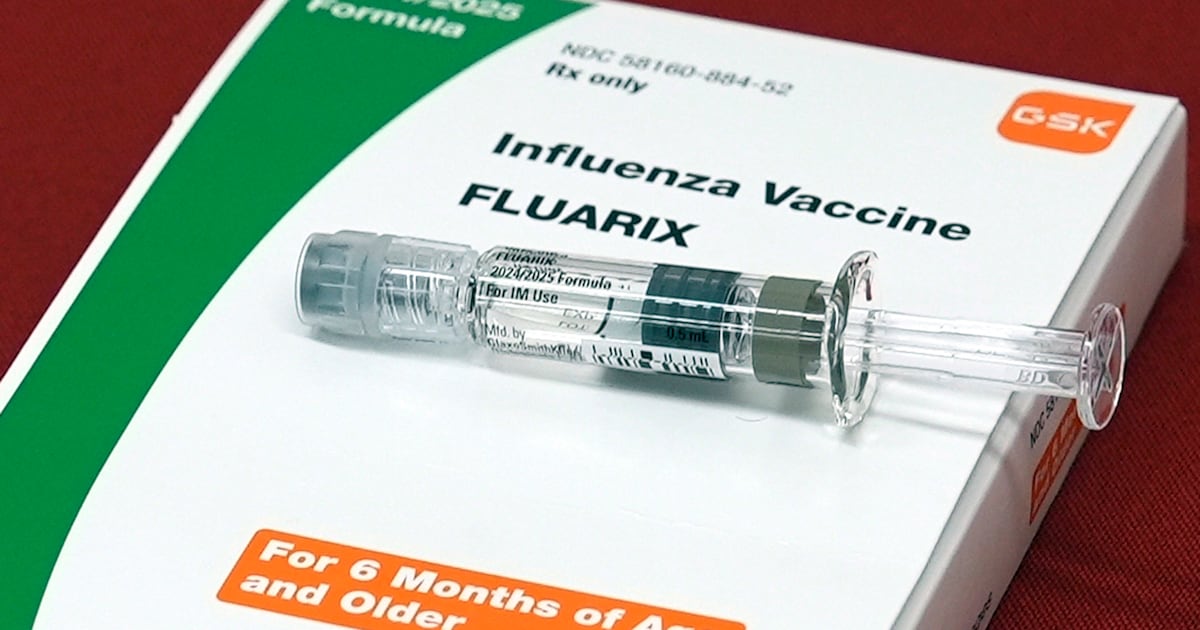
Prevention and What's Next
Vaccination rates hover around 43% for children, with 90% of pediatric deaths among unvaccinated kids.[1][3] Antivirals remain effective against subclade K, and early UK data shows vaccines cutting hospitalizations by 30-75%.[6] Experts predict peak activity lingers for weeks—get vaccinated, wash hands, and stay home if sick to curb spread.[2][5]
About the Organizations Mentioned
CDC
The **Centers for Disease Control and Prevention (CDC)** is the premier national public health agency of the United States, operating under the Department of Health and Human Services and headquartered in Atlanta, Georgia. Its primary mission is to protect public health and safety through disease control, injury prevention, and health promotion both nationally and globally[1][8]. Established in 1946 initially as a single "Center for Disease Control," the agency expanded and reorganized in 1980 into multiple specialized centers, reflecting a broader focus beyond infectious diseases to include environmental health, chronic disease, occupational safety, and health education[7]. The CDC comprises various centers and institutes, such as the National Center for Immunization and Respiratory Diseases, the National Center for Chronic Disease Prevention and Health Promotion, and the National Institute for Occupational Safety and Health (NIOSH), among others. These centers enable the CDC to address a wide array of public health challenges through research, surveillance, policy development, and education[2]. It also plays a key role in emergency preparedness and response, demonstrated notably during the COVID-19 pandemic, where its guidance shaped public health actions despite complex political and social dynamics[8]. Key achievements include pioneering epidemiological research, controlling outbreaks of infectious diseases, advancing vaccine safety and immunization programs, and addressing emerging health threats such as obesity and diabetes. The CDC is recognized for disseminating authoritative health information, including the widely cited Morbidity and Mortality Weekly Report (MMWR), and for its global collaborations with health organizations worldwide[1][3][8]. Currently, the CDC is undergoing organizational adjustments to focus more intensively on infectious diseases, as part of the 2025 Department of Health and Human Services reorganization. This includes absorbing the Administration for Strategic Preparedness and Response while shifting some functions like occupational safety to new entities[1]. The agency’s comprehensive approach, backed by science and government funding, positions it as a critical leader in public health innovation, disease prevention, and health security i